Indications for PGD
Indications for PGD are:
- recurrent miscarriages
- more than 2 unsuccessful IVF cycles
- unexplained infertility
- advanced maternal age
- male factor infertility
- history of chromosomally abnormal child or pregnancy
- chromosomal translocations
- family history of a structural chromosomal condition
- family history of the x-linked disease
- inherited genetic disorders
- reduce genetic risk factors
- single gene disorders
- late on-set disorders
- inherited predisposition to cancer
- HLA matching
Recurrent Miscarriage & Infertility
PGD dramatically improves the chance of a successful IVF pregnancy in couples where prior IVF failures have remained unexplained.
Most IVF centres look very closely at the appearance of embryos under the microscope, as they attempt to determine a "good" or "high quality" embryo from those of lesser quality.
Recent advances have shown, however, that even embryos receiving the highest ratings from scientists because of their "normal" or "excellent" appearance under the microscope may in fact be highly abnormal and completely incapable of ever producing a pregnancy. This discovery was brought about by the addition of preimplantation genetic diagnosis (PGD) to the tools available to scientists in the IVF laboratory.
PGD has offered physicians and scientists, for the first time ever, the ability to examine far beyond the superficial appearance of an embryo. We are now able to examine the most important internal genetic code of the embryo as well. And with these new genetic tools, we have come to learn that some embryos that appear on the surface to be of the highest quality may carry a genetic code that makes them poor choices for attempting to establish a healthy pregnancy.
We have also now learned that other embryos that might have been classified as less than optimal based on their appearance, and may not have been selected for return to the mother may in fact be of the finest quality and have ten or twenty times more chance of producing a healthy pregnancy than those that would have been selected without the use of the remarkable new PGD tools. That beauty in an embryo is more than skin deep, has now been confirmed by science. The technique has also allowed confirmation, for the first time, of the suspicions of our IVF scientists that simply observing and grading the appearance of an embryo may fall far short of being able to provide reliable information to patients who have failed IVF.
PGD is helpful for patients with unexplained infertility, recurrent miscarriages, unsuccessful IVF cycles, advanced maternal age, or male factor infertility. In those cases, the most likely cause is a chromosome abnormality.
Chromosome abnormalities include aneuploidy and structural abnormalities. Aneuploidy is the most common chromosomal abnormality. Aneuploidy can occur in both eggs and sperm. Structural abnormalities include translocations, inversions, and deletions. Structural chromosome abnormalities can also be present in eggs and sperm.
The transmission of a chromosome abnormality to an embryo can result in a low implantation rate, miscarriage or the birth of a baby with a genetic disorder. Using Fluorescence In Situ Hybridization (FISH), the scientists in our PGD laboratory can identify the absence of these specific genetic disorders in each normal developing embryo. As a result, only those embryos free of genetic disease will be transferred to the patient’s uterus so as to increase the chance of conception and ultimately a healthy baby.
Free Online Consultation with Dr Thanos Paraschos and his team
More than 2 unsuccessful IVF Cycles
In vitro fertilization (IVF) frequently enables couples with infertility to achieve successful pregnancies. Some couples, even after numerous IVF attempts, are unable to become pregnant. Some cases of IVF failure are due to the transfer of embryos with chromosome abnormalities. PGD for aneuploidy minimizes the likelihood of a chromosome abnormality in a future pregnancy and increases the chance of achieving an ongoing successful pregnancy.
Unexplained infertility
The most probable cause of unexplained infertility or history of habitual miscarriage is a chromosome abnormality. The male or female partner may be a carrier of a translocation or be an aneuploid mosaic.
Advanced maternal age
Women of advanced maternal age (≥ 37) are at a higher risk of producing aneuploid embryos, resulting in implantation failure, a higher risk of miscarriage or the birth of a child with a chromosome abnormality (e.g. Down syndrome). This is due to the fact that all of the woman's eggs are present at birth. Over time, the chromosomes within the egg are less likely to divide properly, resulting in cells with too many or too few chromosomes.
Aneuploidy is also believed to be a major reason for the decrease of fertility with age. Several studies have determined that approximately 70% of embryos from women of advanced maternal age may be aneuploid. For women aged 37 years and older undergoing IVF, PGD for aneuploidy significantly improves pregnancy rates, reduces miscarriage rates, and decreases the chance of a chromosomally abnormal pregnancy if six or more embryos of good quality are available for analysis.
Male factor infertility
Approximately one-half of all infertility is caused by sperm abnormalities. Many sperm disorders are due to a chromosome abnormality such as aneuploidy or a structural chromosome abnormality. Men carrying a balanced translocation chromosome are at risk of producing sperm with a structural chromosome abnormality.
Several studies have determined that approximately 3-8% of sperm from normal, fertile men are aneuploid and 27-74% of sperm from men with severe infertility are aneuploid. Couples with infertility due to male factor, should consider chromosome analysis on the males sperm prior to IVF.
History of chromosomally abnormal child or pregnancy
For patients with a previous child or pregnancy with a chromosomal abnormality, PGD can reduce the risk of certain abnormalities in the patient’s next pregnancy. This may be an attractive alternative to CVS or amniocentesis for some people, as they may be able to avoid termination of an abnormal pregnancy.
Family history of structural chromosomal condition
For patients with a previous child or pregnancy with a chromosomal abnormality, PGD can reduce the risk of certain abnormalities in the patient’s next pregnancy. This may be an attractive alternative to CVS or amniocentesis for some people, as they may be able to avoid termination of an abnormal pregnancy.
Family history of X-linked disease
A category of monogenic diseases has an X-linked inheritance. Most couples at risk for an X-linked condition are identified by review of the family history or the birth of an affected child. X-linked conditions are caused by a change, or mutation, in a gene on the X chromosome and typically affect only males. This is because males have only one X chromosome, inherited from their mother, while they get a Y chromosome from their father. Since a male has only one X chromosome, if it has a mutated gene he will develop the disorder. It is this type of inheritance that causes disorders such as Duchenne Muscular Dystrophy, Hemophilia, Fragile X, etc.
Females are usually not affected because they have two X chromosomes. Females with one normal X chromosome and one mutated X chromosome generally do not have symptoms of the disease because of the presence of the normal gene. These females are referred to as “carriers” and are at risk for passing on the gene mutation to their children. If that child is a girl who inherits the gene, she also will be a carrier. Once the sex of the embryo is determined, female embryos, which would not be at risk for a sex-linked disorder, would be transferred.
Inherited genetic disorders
Couples at high risk of transmitting an inherited disease to their offspring, have the option of undergoing prenatal diagnosis to allow the detection of the genetic disorder in fetus. However, if the analysis reveals a genetically affected fetus the only options available to couples are to have a child with a genetic disease or to terminate the affected pregnancy. This is a difficult and often traumatic decision, especially in advanced pregnancies.
Many couples may also experience repeated pregnancy terminations in attempts to conceive a healthy child and might feel unable to accept further affected pregnancies. In some cases this may also not be a viable option for religious or moral reasons.
Preimplantation genetic diagnosis (PGD) has been introduced as an alternative to prenatal diagnosis, to increase the options available for couples who have a known genetically transmittable disease, providing reassurance and a reduced anxiety associated with reproduction. PGD can be considered as a very early form of prenatal diagnosis. Its intended goal is to diagnose a specific genetic disease on oocytes or embryos before a clinical pregnancy has been established, by selecting and transferring to the uterus only embryos resulted unaffected after mutation analysis. Consequently, PGD may spare the couple decisions regarding possible pregnancy termination, ensuring a pregnancy free of the disease under consideration.
PGD usually requires that the couple undergoes to an in vitro fertilization (IVF) treatment. This involves hormonal treatments that allow the collection of multiple eggs from the mother. The eggs are then fertilized using the father’s sperm and the resulting embryos are transferred to an incubator. After three days the embryos usually consist of a tiny ball of eight cells, known as blastomeres. To test the blastomere, an opening is made in the covering of the embryo. One or two blastomeres are then removed (biopsied) from each embryo and subjected to genetic testing. If a blastomere is found to be unaffected by the inherited disease then the embryo that it was removed from will also be unaffected. Embryos that are revealed to be healthy can be transferred to the womb, ultimately producing unaffected babies.
Testing of the biopsied cells destroys them because their membranes must be broken open to release the DNA. As such, one cannot use them for any other purpose or return them to the embryo.
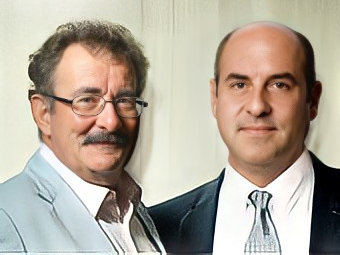
Dr Thanos Paraschos: trained by the Father of PGD, Lord Professor Robert Winston
As a Senior Registrar/Research Fellow to Lord Professor Robert Winston, Dr Paraschos was responsible for organising and implementing the PGD programme to patients at Hammersmith Hospital, where the first genetic pre-implantation diagnosis in the world was performed on an embryo.

